In this blog, I’ll talk about one of the ways in which you can obtain a catastrophic impairment designation, where as a direct result of your motor vehicle accident the impairment you sustained – if you are an adult – results in a traumatic brain injury.
A catastrophic impairment designation places you – an auto accident victim – in the highest level of impairment category available under automobile insurance regulations. While not a benefit itself, a catastrophic impairment designation is the gateway or vehicle to access enhanced benefits, where your policy limits increase to $1 million. All other impairments fell under the non-catastrophic and minor injury category.
If you want to learn more about the companion accident benefits claim, and kickstarting the accident benefits application process, then please click the “link” to read my blog entitled “How to Get Your Accident Benefits Application Started”.
The June 1, 2016 amendments to the Ontario Regulation 34/10: Statutory Accident Benefits Schedule (SABS 34/10), issued under the Insurance Act, R.S.O. 1990, c. I.8, introduced a stricter definition of catastrophic impairment. Section 3.1 was added to the SABS 34/10, which provides a tightening of the criteria for determination of catastrophic impairment.
One of the changes was the introduction into the SABS 34/10 of the use of the Extended Glasgow Outcome Scale for the determination of the overall social outcome, inclusive of psychological, mental, and neurological disabilities of function, of an adult who suffered a traumatic brain injury .
The stricter definition of catastrophic impairment as it relates to a loss of vision in both eyes can be found subsection 3.1(1)4 of the SABS 34/10, as amended by Ontario Regulation 251/15, reads as follows:
For the purposes of this Regulation, an impairment is a catastrophic impairment if an insured person sustains the impairment in an accident that occurs on or after June 1, 2016 and…:
- If the insured person was 18 years of age or older at the time of the accident, a traumatic brain injury that meets the following criteria:
-
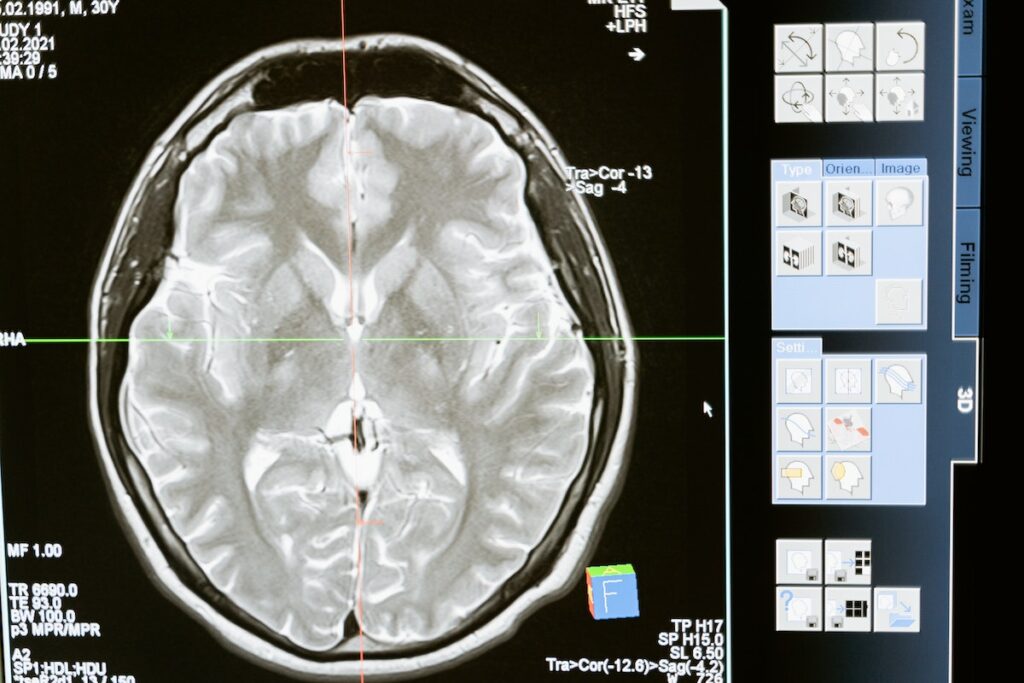
- The injury shows positive findings on a computerized axial tomography scan, a magnetic resonance imaging or any other medically recognized brain diagnostic technology indicating intracranial pathology that is a result of the accident, including, but not limited to, intracranial contusions or haemorrhages, diffuse axonal injury, cerebral edema, midline shift or pneumocephaly.
- When assessed in accordance with Wilson, J., Pettigrew, L. and Teasdale, G., Structured Interviews for the Glasgow Outcome Scale and the Extended Glasgow Outcome Scale: Guidelines for Their Use, Journal of Neurotrauma, Volume 15, Number 8, 1998, the injury results in a rating of,
- Vegetative State (VS or VS*), one month or more after the accident,
- Upper Severe Disability (Upper SD or Upper SD*) or Lower Severe Disability (Lower SD or Lower SD*), six months or more after the accident, or
- Lower Moderate Disability (Lower MD or Lower MD*), one year or more after the accident.
Criteria for Catastrophic Determination
Therefore, if you are at least 18 years of age or older at the time of your MVA and suffered a traumatic brain injury, then in order for you to be granted a catastrophic impairment designation, you must satisfy the aforementioned three criteria:
- Positive findings of “intracranial pathology” as a result of the accident;
- The findings of intracranial pathology must be from a “medically recognized brain diagnostic technology”; and
- When assessed in accordance with the Glasgow Outcome Scale (GOS) and the Extended Glasgow Outcome Scale (GOSE), the traumatic brain injury is rated as either a vegetative state at least one-month post-MVA, an upper or lower severe disability at least six months post-MVA, or a lower moderate disability at least one-year post-MVA.
A Bit of History of the GOS and GOSE
In order for you to have a full appreciation of the criteria, it would be helpful for you to have a bit of history of the GOS, followed by a better understanding of the structured interviews used for the GOS and the GOSE, the guidelines for their use in the comparative assessment of traumatic brain injuries in adults, and the method of rating them.
Of note, is that in the 2011 Superintendent’s Report on the Definition of Catastrophic Impairment in the Statutory Accident Benefits Schedule, which made recommendations to the Minister of Finance that influenced Ontario Regulation 251/15, one of the recommendations was that insureds be evaluated for a rating of a vegetative state based on the GOSE 3 months after the accident. However, the Superintendent of Financial Services concluded that the evaluation for a rating a vegetative state based on the GOSE can commence one month after the accident.
Lastly, the Superintendent of Financial Services accepted the recommendation of the expert medical panel to eliminate the Glasgow Coma Scale (GCS) as a measurement tool to determine a catastrophic impairment in adults with traumatic brain injuries because of the following:
…it has proven a poor tool for predicting the long-term outcomes of traumatic brain injury. In addition, the GCS has weaknesses because it relies on a claimant’s ability to communicate. Hence, inaccurate scores may result with patients who have alcohol in their blood, have breathing tubes inserted or are too young to understand verbal cues.
Under the older Ontario Regulation 403/96: Statutory Accident Benefits Schedule (SABS 403/96), you could’ve been deemed catastrophically impaired, if in accordance with subs. 2.(.1)(e)(i) you sustained a brain impairment as a direct result of your accident, which resulted in the following:
a score of 9 or less on the Glasgow Coma Scale, as published in Jennett, B. and Teasdale, G., Management of Head Injuries, Contemporary Neurology Series, Volume 20, F.A. Davis Company, Philadelphia, 1981, according to a test administered within a reasonable period of time after the accident by a person trained for that purpose.
The Superintendent of Financial Services, however, did accept the expert medical panels’ recommendation to replace the GCS with the GOSE, because as an outcome-based measurement tool it is much more accurate, effective, and predictable of the outcome of a traumatic brain injury.
The Glasgow Outcome Scale
Jennett et al. noted that the original GOS, or the expanded version known as the GOSE, “allows the overall social outcome of most patients to be assessed reliably on the basis of a structured interview which concentrates on social and personal functioning, without the need for detailed neurological and psychological evaluation”. Therefore, the GOS enables qualified assessors to ascertain the degree of disability and the net effect of all the separate disabilities on the ability to function, in the absence of examining the specific contributing factors to the disability of function.

The Purpose of the Glasgow Outcome Scale
Wilson et al. identified the purpose of the development of the GOS as being the following:
… to allocate people who have suffered acute brain damage from head injury or nontraumatic insults into broad outcome categories. The scale reflects disability and handicap rather than impairment; that is, it focuses on how the injury has affected functioning in major areas of life rather than on the particular deficits and symptoms caused by injury (World Health Organization, 1980). It is not intended to provide detailed information about the specific difficulties faced by individual patients, but to give a general index of overall outcome. It is of particular value in allowing the outcome of different groups of patients to be compared in a simple and easily interpreted fashion (Marshall, 1987). It has been recommended as a measure of outcome for clinical trials (Clifton et al., 1992) and has been widely adopted for this purpose.
Again, the GOS is not intended to provide the specific factors that contribute to your disability in function, but rather provide a general index of the net effect of the disabilities on your overall outcome.
Overall Outcome
Many victims of motor vehicle accidents, such as yourself for example, will sustain severe head injuries and face many years of disability, which will negatively impact your mental and physical function. Jennett noted that “Although the separate components of handicap after brain damage have frequently been described, particularly those which can be measured by psychometric tests, what matters to the patient is the net effect of all his separate disabilities on his functioning as a person, which includes the extent of his dependency on others”, which they “termed the overall social outcome”. Therefore, what is meant by outcome is the overall social outcome, which is inclusive of the total effect of all the victim’s psychological, mental and neurological disabilities of function. More importantly, this overall social outcome is what the GOS measures via the scale that comprises four outcomes or categories.
Vegetative State: No Meaningful Responsiveness
The first outcome or category is the vegetative state, which is a non-sentient state where a survivor of a severe brain injury shows no evidence of meaningful responsiveness. If you are capable of complying with simple commands or saying simple words, then you would be upgraded to the severe disability category. Jennett et al. noted the following concerning a vegetative state:
Vegetative patients breathe spontaneously, have periods of spontaneous eye-opening when they may follow moving objects with their eyes, show reflex responses in their limbs (to postural or painful stimuli), and they may swallow food placed in their mouths. This non-sentient state must be distinguished from other conditions of wakeful, reduced responsiveness – such as the locked-in syndrome, akinetic mutism and total global aphasia. Although the vegetative state indicates lack of function in the cerebral cortex, this may be structurally intact; for this reason Jennett and Plum argued that the term “apallic syndrome” was inappropriate.
Therefore, if you fall into this category, then you would not be able to perceive or feel things, obey even simple commands, or utter or communicate.
Severe Disability: Conscious but Dependent
The second outcome or category is severe disability, where a survivor of a severe brain injury is conscious and sentient, but requires the continuous aid of another person to do some of his or her activities of daily living every day, which he or she would’ve otherwise done independently. Jennett et al. noted the following concerning a severe disability:
This may range from continuous total dependency (for feeding and washing) to the need for assistance with only one activity – such as dressing, getting out of bed or moving about the house, or going outside to a shop. More often dependency is due to a combination of physical and mental disability – because when physical disability is severe after a head injury there is almost always considerable mental deficit. But a few patients who have little or no physical deficit are unable to organize their day-to-day lives effectively, and must be classified as severely disabled. The worst of these requires the care and protection which only a mental hospital can provide, while others cope at home with the support of attentive relatives, but could not be left overnight because they would be unable to plan their meals or to deal with callers, or any domestic crisis which might arise.
Therefore, if you fall within the severe disability outcome category, then you are conscious and sentient, but are totally dependent on at least one other person.
Moderate Disability: Independent but Disabled
The third outcome or category is moderate disability, where a survivor of a brain injury is independent without the need for continuous aid of another person to do some of his or her activities of daily living every day, but due to his or her mental disability, or a combination of a mental and physical disability, he or she cannot do some of his or her activities of daily living. Jennett et al. noted the following concerning a moderate disability:
Such a patient is able to look after himself at home, to get out and about to the shops and to travel by public transport. However, some previous activities, either at work or in social life, are now no longer possible by reason of either physical or mental deficit. Some patients in this category are able to return to certain kinds of work, even to their own job, if this happens not to involve a high level of performance in the area of their major deficit.
Therefore, if you fall within the moderate disability outcome category, then you are independent, but disabled in some, but not all, of your previous activities.
Good Recovery: Normal Capacity
The fourth outcome or category is good recovery, where a survivor of a brain injury resumes the capacity to fully engage in his or her pre-accident, normal activities of daily living, inclusive of social, work, house and leisure activities, but still suffers minor mental or physical deficits, or a combination of both. Jennett et al. also noted that “…for various reasons, the patient may not have resumed all his previous activities, and in particular may not be working”. Therefore, if you fall within the good recovery outcome category, then you are either independent, or via successful rehabilitation or alternative therapeutic measures, you recover enough from your brain injury to resume your normal activities of daily living, albeit with some limitations.
The GOS is internationally recognized and the most extensively used scale by clinicians to both assess and measure the outcome or after-effect of a traumatic brain injury and non-traumatic causes of brain injury. However, over time clinicians began to identify significant limitations and shortcomings of the traditional GOS, which were eventually addressed by adopting a set of guidelines for the use of a standardized format for structured interviews of patients with brain injuries, and identifying specific criteria for assigning an outcome category, in order to enhance the reliability of the assessment and measurement of the outcome.
Fixing the Shortcomings and Limitations of the Old GOS
The traditional format of the GOS was a great foundation to build upon, but it did have shortcomings and limitations that needed to be addressed. The short interview of the old format lacked structure and was open-ended, which fostered subjective reactions presented unsystematically from the assessors. The application of the old format resulted in an interpretation of the GOS as giving special importance to physical limitations as opposed to cognitive and emotional limitations. The old format had a lack of guidelines for dealing with problems such as, but not limited to, “extracranial injury, epilepsy, and preinjury unemployment”. The broadness of the GOS outcome categories of the old format made it difficult for the assessor to note subtle changes in the patient’s functional status.
Wilson et al. approached overcoming the aforementioned shortcomings and limitations of the traditional GOS by doing the following:
…adopting a standard format for the interview and identifying specific criteria for assigning an outcome category. The major categories of outcome used in the present structured interviews follow closely the descriptions of the Glasgow Outcome Scale provided by Jennett and Bond (1975), Jennett et al. (1981), and Jennett and Teasdale (1981). The questionnaires are designed to achieve greater objectivity and reliability than the traditional method of assigning an outcome category.
Wilson et al. created a set of guidelines for assessors to conduct structured interviews for the GOS, especially in areas that require the exercise of judgment and are therefore susceptible to subjective reactions presented unsystematically. These guidelines are captured in four rules for the application of the GOS.
The Four Rules for the Application of the GOS
The first rule is “Disability due to head injury is identified by a change from preinjury status”, which requires an assessment of your preexisting disability that constituted your baseline. This is necessary in order to better isolate and assess the specific changes and disability that have occurred as a direct result of your head injury. The second rule is “Only preinjury status and current status should be considered”, which requires the assessor to focus on the level reached as a result of your current or present status approximately over the past week. Therefore, the assessor is to consider irrelevant to a determination of outcome, the original severity of your head injury at the time it occurred or your optimistic view of your future level and recovery. The third rule is “Disability must be a result of mental or physical impairment”, which requires the assessor to probe deeper to ascertain what specific activities the patient is capable of performing even if they do not actually do it, and specific activities the patient is incapable of doing as a result of a mental and/or physical impairment caused by the head injury. The fourth rule is “Use the best source of information available”, which in some circumstances requires the assessor to take practical steps to improve the overall quality of information received by not solely relying on your verbal reporting of your head injury, because it may be misleading. Therefore, the assessor is also required to rely on others, such as a caregiver, or a close family member, relative and/or friend.
Other Considerations to Administering the GOS
Wilson et al. also offered other considerations to assessors administering the scale. For example, the risk of epilepsy and its subsequent restrictions on you should not be factored into the determination of your overall GOS score, unless you have actually suffered a seizure. Also, since the GOS is used to determine the effect of brain injuries specifically, the effect of your other non-brain injuries or illnesses should not be factored into the determination of the overall GOS score, unless they are so severe, such as major spinal cord injuries, where it is almost impossible to assign a score that only factors in the effects of the brain injury. If your non-brain injury or illness is so severe that it must be factored in, then it should be noted by the assessor administering the GOS.
The Extended Glasgow Outcome Scale
One of the criticisms of the GOS was that its four aforementioned categories or outcomes that comprise the interview, namely vegetative state, severe disability, moderate disability, and good recovery, were too broad. So, in 1981, Jennett et al. concluded that as a result of the aforementioned four categories being too broad, they were insensitive to degrees of improvement, which made it difficult for the assessor to note subtle changes in the patient’s functional status. Jennett et al. decided that in order to improve the sensitivity to the degrees of improvement, which occurs within each of the three conscious outcome categories (severe disability, moderate disability, and good recovery), it was necessary to divide them into a better and worse level. The result would be a six-point scale for conscious survivors of brain injuries, or six probable outcomes, but when you include the two undivided, unconscious categories of dead and vegetative, then you get an extended eight outcome point scale, or eight probable outcomes. The three aforementioned conscious outcome categories, which were divided into better and worse levels, are expressed in the GOSE questionnaire as “upper” and “lower”.
The ultimate goal of creating a structured set of guidelines for the GOS and GOSE, and refining the questionnaire to obtain greater objectivity and reliability in assessing and determining the net effect of the disabilities on your function, is to enhance the prediction of the overall social outcome. The more the prediction of overall social outcome of survivors of severe brain injuries, such as yourself, is improved in terms of an accurate categorization of the degree of severity, the better that the effectiveness of the management decisions would be pertaining to your treatment and rehabilitation, in general, and your continuous care, in particular . However, one of the keys to increasing the accuracy in predicting overall social outcome, is the timing of the administration of the GOS and GOSE.

The Best Time to Administer the GOS and GOSE to Determine Outcome
Wilson et al. believe that the GOS and GOSE was intended to be used after discharge from the hospital, which is of note because subs. 3.1(1)4 of the SABS 34/10, as amended by Ontario Regulation 251/15, makes it clear that the GOS and GOSE are to be administered at different times after discharge, at: (i) one month, (ii) six months, and (iii) a year or more. Why?
Jennett et al. analyzed the nature of neurological and mental disabilities stemming from severe brain injuries in 150 patients, which overtime manifested in social disability. They found the following important findings, in regards to patients with severe brain injuries:
patients … who were conscious three months after injury were re-assessed later [sic] there were fewer who improved between six and 12 months than between three and six months. Of those who by 12 months had made a good recovery, or who were by then moderately disabled, almost two thirds had already reached this level within three months of injury and 90% had done so by six months. This corresponds with the pattern of recovery for many aspects of cognitive function. Examination of the 150 patients in the present study confirmed that 10% of patients who were severely or moderately disabled at six months were in the next best category by one year. When reassessment was made using the six point scale it was found, as expected, that 20% had improved by one subcategory between six months and 12 months. Only 5% of 82 patients, followed for more than 18 months improved sufficiently after 12 months to reach a better category. It was exceptional for a patient who was severely disabled at three months after injury to ever reach the category of good recovery.
Jennett et al. also discovered that the vast majority of the patients reached their final outcome category within six months of the brain injury, and after a year the number of patients that changed categories was miniscule. This discovery by Jennett et al. explains why in subs. 3.1(1)4 of the SABS 34/10, as amended by Ontario Regulation 251/15, the GOS and GOSE are to be administered at six months and a year after the MVA, in regards to upper and lower severity disability, and the lower moderate disability outcome categories, respectively.
Conclusion
Therefore, if you were 18 years of age or older at the time of your MVA, and was deemed to suffer a traumatic brain injury following:
- A positive finding of intracranial pathology from medically recognized brain diagnostic technology; and
- An assessment of the overall social outcome following your brain injury, in accordance with J. Wilson’s et al.’s aforementioned structured interviews concentrating on social and personal functioning, resulted in a rating of at least one of the following outcome categories:
- Vegetative state, at least one month after the MVA;
- Upper severe disability or lower severe disability, at least six months after the MVA; or
- Lower moderate disability, at least one year after the MVA,
then you would obtain a catastrophic impairment designation in accordance with subs. 3.1(1)4 of the SABS 34/10, as amended by Ontario Regulation 251/15.
Lastly, Wilson et al. noted that the GOS and GOSE are not reliable in its application to young children, as the criteria used can’t be applied. This will be important to keep in mind as a discuss in my blog entitled “Catastrophic Impairment: Paediatric Traumatic Brain Injuries”, the catastrophic impairment definition for children in subs. 3.1(1)5 of the SABS 34/10, as amended by Ontario Regulation 251/15, which will include a discussion of the application of the King’s Outcome Scale for Childhood Head Injury.
Additional Resources
Provincial
Ontario Brain Injury Association
The Ontario Brain Injury Association (OBIA) is a “provincial head injury association because health care, housing and service provision issues related to brain injury were largely provincial matters”. They offer a wide array of useful resources, which range from concussion resources for both adults and resources, statistical information on acquired brain injuries (ABI), caregiving after a brain injury, and the learning needs of children with disabilities during COVID-19, to educating educators about ABI, OBIA webinars/seminars, a bookstore, a directory of ABI services and finding a qualified trauma lawyer such as myself. Please visit their website for more information at the following URL address:
National
Brain Injury Canada
The Brain Injury Canada is a “national charitable organization focused on education, awareness, and advocacy for the brain injury community”. They have a great resource website with an interactive service directory, which is designed for the brain injury community, and gives you access to the new services, organizations and associations that over acquired brain injury and traumatic brain services, as well as many other resources. Their website is “overseen by a Scientific Advisory Committee of physicians, clinicians and researchers from across Canada”. They support “those living with acquired brain injury, their families/caregivers and health care professionals by providing current, evidence-based information about brain injury, treatment, rehabilitation and recovery”. Please visit their website for more information at the following URL address:
https://braininjurycanada.ca/en/node/3
March of Dimes Canada’s Brain Injury Services
March of Dimes Canada’s Brain Injury Services “provides experienced and flexible care for people dealing with the effects of brain injury”. They “offer rehabilitation and social support services” and their goal is to help you “regain your purpose and become as independent as possible”. They are the “largest national organizations for people living with disability in Canada”. Please visit their website for more information at the following URL address:
https://www.marchofdimes.ca/en-ca/programs/abi
Toronto
Toronto Acquired Brain Injury Network
The Toronto Acquired Brain Injury Network “helps hospitals and community-based programs connect people with Acquired Brain Injury (ABI) to the services they need”. They work with their “members and other stakeholders to improve the quality and availability of publicly funded ABI services and support”. Further to their mission statement, they “provide leadership in furthering equitable, accessible, responsive, cost-effective and quality publicly-funded services and support for persons living with the effects of an acquired brain injury in the Greater Toronto Area”. Please visit their website for more information at the following URL address:
Cota Health
Cota Health is “an accredited, not-for-profit, community-based organization that has been supporting adults with mental health and cognitive challenges to live well within their communities for over 45 years”. They “provide person-centred supports that assist individuals to find inspiration and hope in their inherent strengths and support them to pursue meaningful change in their lives, as they define it”. They work collaboratively with their funders, partners and other stakeholders “across the provincial health and social service systems, to inspire positive change in the way that services are delivered to individuals living with mental health and cognitive challenges”. They “offer a wide range of services to adults living with serious mental illness, geriatric mental health conditions, acquired brain injuries, developmental disabilities and dual diagnoses”. Their “services include case management, supportive housing, short-term residential beds, day programs, court and justice related services, an Assertive Housing First Team (AHFT) and services for individuals who are experiencing homelessness”. Please visit their website for more information at the following URL address:
West Park Healthcare Centre – Adult Day Program
The West Park Healthcare Centre’s Adult Day Program “provides social and educational activities, and community outings”, as well as “community case management to clients and families, overnight respite, and consultation with a physiatrist”. They recognize that people “who have sustained a severe acquired brain injury (ABI) may experience social isolation and place significant burden on family members due to impairments and challenging behaviours that prevent survivors from living independently”, which they try to alleviate with this program. Please visit their website for more information at the following URL address:
https://www.westpark.org/en/Services/ABIAdultDayProgram
UHN Toronto Rehabilitation Institute – Acquired Brain Injury Rehab Services
The UHN Toronto Rehabilitation Institute – Acquired Brain Injury Rehab Services “provides outpatient care at both the University Centre and Rumsey Centre”, which require a referral. They recognize that “a brain injury can be devastating and may lead to trouble in cognitive ability, moving, balance, coordination, speech and language, or behavioural and emotional problems”. They also provide “rehabilitation to people who have acquired non-degenerative neurological disorders”, and they “help those with a brain injury work towards returning to work and to living more independently”. Their rehabilitation programs are tailored to “an individual’s needs and focus on bringing back functions that can be restored” and if that’s not possible, then they “teach people how to do things differently”. Please visit their website for more information at the following URL address:
https://www.uhn.ca/TorontoRehab/Clinics/Brain_Injury_Services
SunnyBrook Hospital – Neuropsychiatry Program
SunnyBrook Hospital’s Neuropsychiatry Program “offers a comprehensive clinical service to patients who have psychological difficulties secondary to neurological illness”. Even though their “main clinical focus centres on patients with multiple sclerosis, traumatic brain injury and Conversion Disorder, expertise is available across the whole spectrum of neuropsychiatric disorders”. Their comprehensive “Assessments include detailed brain imaging and cognitive (neuropsychological) testing” and they have “a strong research component that complements the clinical focus (i.e., MS, TBI and Conversion)”. Please visit their website for more information at the following URL address:
https://sunnybrook.ca/content/?page=psychiatry-neuropsychiatry-program
St. Michael’s Hospital, Neurocognitive Evaluation and Rehabilitation Head Injury Clinic
St. Michael’s Hospital, Neurocognitive Evaluation and Rehabilitation Head Injury Clinic “is the largest of its kind in Ontario with 2,000 patient visits per year”. It provides “assessment, diagnosis and management of physical, cognitive and behavioural/psychological symptoms for patients who have sustained mild and moderate traumatic brain injury (mTBI)”. It’s “run by a multidisciplinary team including physiatrists, neuropsychiatrist, neuro-otolaryngologist, RN clinical coordinator, social worker, cognitive speech-language pathologist, and research associate”.
Further to their website, their goals include: (1) “Early Assessment, diagnosis and comprehensive medical management (pharmacological and non-pharmacological) of TBI and related disability”; (2) “Coordination of community supports and rehab services”; (3) “Provide reintegration support for patients returning to work/school”; (4) “Collaborate with other providers across the system to best meet patient’s needs (OHIP and third party-funded services)”; (5) “Provide education related to mTBI to patients /family to guide them in their recovery”; and (6) “Serving a unique patient population”. You require a referral “directly from the Trauma Neurosurgery Department, Emergency Department and Family Practice at St. Michael’s”.
Please visit their website for more information at the following URL address:
Outside Toronto
Hamilton Health Sciences’ Acquired Brain Injury Outpatient Clinic and Services
Hamilton Health Sciences’ Acquired Brain Injury Outpatient Clinic and Services “sees individuals with severe, moderate and mild brain injury”, who “usually live at home or in community facilities”. They focus “on assessment and problem solving for individuals with known or suspected brain injuries”. They address needs, such as, but not limited to, the following: (1) “Assistance in accessing existing community resources (such as occupational therapy, physiotherapy, counseling, life skills programs, recreational programs, substance treatment services, vocational re-entry services, driving assessment services)”; (2) “Education about brain injury and the impact on functional abilities (such as mobility, self-care, communication)”; (3) “Rehabilitation medical management”; (4) “Medication management”; and (5) “Neuropsychiatric treatment”. Please visit their website for more information at the following URL address:
Head Injury Rehabilitation of Ontario (HIRO)
The Head Injury Rehabilitation of Ontario (HIRO) provide support to people with “moderate to severe acquired brain injury (ABI) in the community and provide a promise of hope and a path forward after an ABI”. HIRO is “unique in its ability to provide evidence-based, client and family centered ABI rehabilitation care in the community”. Further to their website, they “work with clients and their families to achieve goals that are meaningful for them throughout our continuum of care; from six residential care homes, to transitional living apartments and to community services including group as well as outreach”. They serve people from “across Ontario through services in Hamilton, Burlington, Niagara, St. Catharines, Brant and Haldimand-Norfolk regions”. Their “rehabilitation program is tailored to fit the needs of the client and supported by a network of clinical professionals, care workers, family, friends and community advocates who help facilitate transitions toward greater independence”. Their goal is to help their clients “realize their full and unique potential”. Please visit their website for more information at the following URL address:
Peel, Halton, and Dufferin Acquired Brain Injury Services
Peel, Halton, and Dufferin Acquired Brain Injury Services offers “Community-based support and rehabilitation services to adults living with the effects of an acquired brain injury” and referrals to other community services. Their services include, but are not limited to, the following: assisted living services, caregiving/family services; case management services; clinical services, concussion services, a day program for adults, support of independent living services, and senior services, plus an “Extendicare Halton Hills Integrated Partnership” which supports “clients in need of long-term residency who are at risk of losing residential placement due to cognitive or behavioral challenges”. Please visit their website for more information at the following URL address:
https://peel.cioc.ca/record/MHL0082
York-Simcoe Brain Injury Services
York-Simcoe Brain Injury Services has established a “partnership between Mackenzie Health and March of Dimes Canada” in order to provide “case coordination and comprehensive functional behavioural assessment to evaluate the effects of brain injury”, where “an individualized service treatment plan is developed with recommendations and community support to promote acquisition of skills and strategies for reintegration” at “Mackenzie Health, through York-Simcoe Brain Injury Services”, which “also offers Adult Day Programs for people with acquired brain injuries at three locations within York Region”. Please visit their website for more information at the following URL address:
https://www.centralhealthline.ca/displayservice.aspx?id=132052
Resources for Acquired Brain Injury and Addiction
Community Head Injury Resource Services (CHIRS) of Toronto
Community Head Injury Resource Services (CHIRS) of Toronto is “a registered not-for-profit charitable organization primarily funded by the Central Local Health Integration Network (LHIN) and by the Ontario Ministry of Health and Long-Term Care”. Further to their website, their mission is “to improve the quality of life for persons living with the effects of Acquired Brain Injury”. Their vision is “to be leading-edge in the provision of evidence-based community and client-centered services in the field of Acquired Brain Injury”. Please visit their website for more information at the following URL address:
Concurrent Disorders Support Services – Fred Victor
Concurrent Disorders Support Services – Fred Victor is “the lead agency in this agency referral network for people with both substance use issues and other mental illness and complex needs in the City of Toronto”. They offer “a high-degree of support to its clients by helping them fast-track and navigate the system”. In order to apply, you must complete the application online at cdss-fredvictor.org. You fax the consent form – available at https://www.fredvictor.org/wp-content/uploads/2020/02/CDSS-Consent-Form.pdf – to (416) 364-8526. They’ll contact you within three business days to discuss service needs.
For more information, you can email cdss@fredvictor.org or call (416) 364-8228 ext. 3365.
In order to be eligible, you require a “referral from a medical practitioner or community-based agency that is working with an individual”. Please visit their website for more information at the following URL address:
https://www.fredvictor.org/what-we-do/health-services/concurrent-disorders-support-services/
Acquired Brain Injury Support Groups
Brain Injury Association of Peel and Halton (BIAPH)
Brain Injury Association of Peel and Halton (BIAPH) “is a non-profit organization which advocates for the needs and provides information to survivors of Acquired Brain Injuries, their families and support network”. They “facilitate measures to promote the prevention of brain injury, improve quality/care of life, provide community education, and conduct resource searches on behalf of our members”. Further to their website, their mission is to “enhance the quality of life for persons in the region(s) of Peel and Halton who are living with the effects of an acquired brain injury through: Education, Awareness and Support”. Please visit their website for more information at the following URL address:
Brain Injury Society of Toronto (BIST)
The Brain Injury Society of Toronto (BIST) “is a community non-profit supporting those living with the effects of acquired brain injury”. Their members are “children, young adults, parents, spouses, grandparents, professional and service providers”, and “Membership is open to anyone”. Further to their website, their mission “is to enhance the quality of life for people in the City of Toronto, living with the effects of acquired brain injury through education, awareness, support and advocacy”. Please visit their website for more information at the following URL address:
Please keep in mind that these aforementioned services may or may not be regulated in Ontario. You can contact the Consumer Protection Ontario to help you ask the right questions before you choose any of their services. If you have a concern or serious complaint about any non-regulated service, then please visit www.ontario.ca/page/consumer-protection-ontario/ for further information.
I hope you found this information valuable. Rudder Law Group’s website is your one-stop source for answers to all of your legal questions concerning catastrophic impairment law and personal injury law.





Leave A Comment